As children return to school, there’s an increased risk of them contracting the Coronavirus. Keep reading to learn how to spot the signs of COVID-19 in children and explore appropriate treatment and dietary approaches.
1. When to Suspect Your Child is at Risk of COVID-19 Infection
Fever coupled with respiratory symptoms such as cough, sore throat, or difficulty breathing, along with any of the following epidemiological factors related to COVID-19, should raise concern:
- History of travel to/from/through epidemic areas (places with confirmed COVID-19 cases or active outbreaks) within 14 days before the onset of symptoms.
- History of exposure to a COVID-19 patient or close contact with suspected cases within 14 days before the onset of symptoms. This includes:
- Exposure to healthcare workers infected with COVID-19 in medical facilities.
- Visiting or sharing a room with a COVID-19 patient.
- Direct contact (within a range of ≤ 2m) with suspected or confirmed COVID-19 cases.
- Living in the same household as a suspected or confirmed COVID-19 case during their illness.
- Attending the same class (nursery, school, etc.) as a COVID-19 patient or suspected case.
- Traveling or socializing with COVID-19 patients or suspected cases.
- Sharing a means of transportation (sitting in the same row, two rows in front, or two rows behind) with a suspected or confirmed COVID-19 case.
- Hospitalized children with symptoms and manifestations of acute respiratory infection of unknown cause.
- Children with a positive SARS-CoV-2 test via rapid testing.
 When to Suspect Your Child is at Risk of COVID-19 Infection
When to Suspect Your Child is at Risk of COVID-19 Infection
2. Signs and Symptoms of COVID-19 in Children
Incubation Period
Typically, the incubation period ranges from 2 to 14 days, with an average of 4 to 5 days. However, due to the emergence of different variants, this period may vary:
- For the MERS and SARS coronaviruses: The incubation period ranges from 2 to 11 days.
- For the new variant: The incubation period is 2 to 14 days, with an average of around 5 days. During this time, the virus can still be transmitted to others.
 Different Variants May Have Different Incubation Periods
Different Variants May Have Different Incubation Periods
Onset Symptoms
- Fever
- Fatigue
- Dry Cough
- Headache
- Sore Throat
- Nasal Congestion/Runny Nose
- Loss of Taste/Smell
- Nausea, Diarrhea, and Muscle Pain
- Less common symptoms: Heart rhythm disturbances, Skin lesions (palmar-plantar erythrodysesthesia, rash…), Hepatomegaly, Hepatitis; Encephalopathy (seizures, coma, or encephalitis), etc.
However, many children may be asymptomatic. Most children only experience mild respiratory symptoms such as low-grade fever, cough, sore throat, runny nose, and fatigue…, and recover within 1-2 weeks. Only about 2% of children experience severe progression by day 5-8.
Factors indicating a potentially severe prognosis: developmental delay, cerebral palsy, chronic lung disease, obesity, immunodeficiency, diabetes, congenital heart disease, etc.
 Runny Nose is a Sign of COVID-19 in Children
Runny Nose is a Sign of COVID-19 in Children
3. COVID-19 Treatment for Children
According to the United Nations Children’s Fund (UNICEF), for children with mild illness treated at home without medication, the following should be noted:
- Isolating the child in a separate room, or following home isolation guidelines provided by the Ministry of Health.
- Applying standard precautions, including wearing masks for children aged 2 years and above.
- Providing ample fluids or oral rehydration solutions to the child.
- Ensuring the child receives adequate nutrition or breastfeeds as appropriate.
- Maintaining oral, dental, and nasal hygiene for the child.
- Instructing older children to perform in-place exercises and breathing exercises for at least 15 minutes per day.
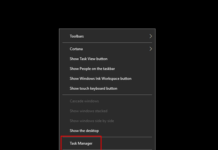
- Monitoring the child’s condition: Taking the body temperature at least twice a day or whenever the child has a fever. Measuring SpO2 levels at least twice a day or whenever the child feels tired, breathes rapidly, or experiences shortness of breath. Fully complying with medical declarations via telephone or applications.
 Take Your Child’s Temperature at Least Twice a Day
Take Your Child’s Temperature at Least Twice a Day
Immediately notify medical staff if any of the following abnormal symptoms occur:
- Fever above 38 degrees C.
- Older children complaining of shortness of breath or chest tightness. Younger children crying inconsolably or exhibiting abnormal behavior.
- Severe sore throat or dry cough.
- Diarrhea.
- SpO2 below 96%.
- Fatigue or lack of interest in play.
- Poor appetite or refusal to breastfeed.
 Inconsolable Crying in Younger Children Warrants Medical Attention
Inconsolable Crying in Younger Children Warrants Medical Attention
For Children Requiring Medication
- Antiviral antibody therapy: Only for children under 12 years of age, weighing 40kg or more, and with risk factors for severe disease progression (underlying medical conditions and no contraindications to the medication). This treatment is only administered in hospitals with the guardian’s consent.
- Casirivimab 600mg + imdevimab 600mg as a single dose. This medication is reserved for children with mild to moderate illness who do not require oxygen support, have been symptomatic for less than 10 days, and meet the above criteria.
Supportive Treatment
- Administer paracetamol at a dose of 10-15 mg/kg/dose every 6 hours and use fever-reducing medications when the temperature rises above 38.5 degrees C.
- Use cough medications, preferably herbal cough remedies.
- Provide vitamin and mineral supplements.
- Manage underlying medical conditions according to established protocols.
 Children Receiving Medication Must Follow Doctor’s Instructions
Children Receiving Medication Must Follow Doctor’s Instructions
For Children Requiring Centralized Isolation
- Ensure constant adult supervision during the isolation period.
- The caregiver must not leave the isolation room or have contact with others.
- Instruct the child on personal hygiene practices, such as handwashing and mask-wearing…
- The caregiver should monitor the health of the child and themselves. If any suspicious symptoms develop, notify medical staff immediately.
- Provide the child with adequate nutrition, encourage fluid intake, and supplement with oral rehydration solutions.
For further reference:
 Instruct Children on Proper Handwashing Techniques
Instruct Children on Proper Handwashing Techniques
4. Nutrition to Boost Children’s Immune System
Consuming a varied and balanced diet helps develop a healthy gut microbiome and strengthens the immune system. Here are some key nutrients to focus on:
Vitamins (A, B6, B12, C, D, E, and K), minerals (iron, zinc, and selenium), and probiotics.
These essential nutrients can be found in the following food groups:
- Milk and cheese: Excellent sources of vitamins A and D.
- Fatty fish: Rich in vitamins A, D, B12, and selenium.
- Green vegetables (spinach, broccoli, kale…): Abundant in vitamins A, B6, folate, and iron.
- Meat and poultry: Contain significant amounts of zinc, copper, and iron.
- Legumes: Great sources of zinc, iron, selenium, vitamin B6, and B12.
- Nuts and seeds: Provide zinc, iron, selenium, vitamin B6, and B12.
- Fruits: Offer vitamins A and C, among other nutrients.
For further reference:
 Green Vegetables Help Boost Children’s Immune System
Green Vegetables Help Boost Children’s Immune System
We hope that through this article, you now know how to recognize the signs of COVID-19 in children and how to manage their treatment and nutrition. Stay tuned for more informative content. Wishing you and your family good health and happiness!
Sources: suckhoedoisong.vn, unicef.org