Being aware of the early signs of miscarriage is crucial, as early detection can help prevent further complications. In this article, we will explore the easily recognizable signs of miscarriage and provide effective prevention methods to reduce the risk.
1. Understanding Miscarriage
 Understanding Miscarriage
Understanding Miscarriage
Miscarriage, or spontaneous abortion, refers to the loss of pregnancy before the 20-week mark. It’s important to know that experiencing a miscarriage does not mean you won’t be able to conceive again. In fact, approximately 87% of women who have had a miscarriage go on to have healthy, full-term pregnancies.
2. Different Types of Miscarriage
 Common Types and Their Symptoms
Common Types and Their Symptoms
Doctors classify miscarriages based on the stage of pregnancy and specific symptoms presented. Here are some of the most common types:
-
Complete Miscarriage: This occurs when all embryonic tissue is expelled from the mother’s body.
-
Incomplete Miscarriage: Some embryonic tissue is expelled, but a portion remains in the uterus.
-
Missed Miscarriage: The embryo stops developing, but the placenta and embryonic tissue are still present in the uterus.
-
Threatened Miscarriage: Characterized by abnormal vaginal bleeding, but the cervix does not dilate. Timely detection and treatment can often save the pregnancy.
-
Infected Miscarriage: This occurs when the uterus becomes infected due to retained embryonic tissue.
3. Uncovering the Causes
 Understanding the Underlying Causes
Understanding the Underlying Causes
Embryonic development relies on a combination of chromosomes from both parents. Issues with either set of chromosomes can lead to abnormalities and miscarriage. These abnormalities may result in conditions such as:
-
Intrauterine Fetal Demise
-
Atretic Follicle
-
Molar Pregnancy
-
Damaged Egg or Sperm Cell
-
Pathology
Additionally, poor self-care or underlying health conditions during pregnancy can increase the risk of miscarriage. These include:
-
Inadequate nutrition or maternal malnutrition
-
Obesity
-
Substance abuse, including alcohol and drugs
-
Thyroid disorders
-
Diabetes
-
Maternal infections or trauma
-
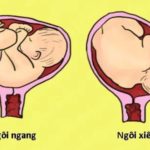
Abnormal uterus shape
-
Severe maternal hypertension
-
Use of certain medications harmful to the fetus
4. Identifying Risk Factors
 Who Is at Risk?
Who Is at Risk?
Several factors can increase the likelihood of miscarriage. These include:
-
Age: The risk of miscarriage rises with maternal age. Statistics indicate a 20% miscarriage rate at age 35, increasing to 40% at age 40 and 80% at age 45.
-
Chronic Illness: Conditions like diabetes and hypothyroidism during pregnancy significantly elevate the risk.
-
Uterine and Cervical Issues: Abnormalities in the cervix or uterus can make miscarriage more likely.
-
Substance Use: Smoking, alcohol, and drug use are significant risk factors.
-
Additionally, invasive prenatal tests, such as amniocentesis and chorionic villus sampling, can increase the risk.
5. Recognizing the Signs
 Signs to Watch Out For
Signs to Watch Out For
Weeks 2–4
During the first few weeks after conception, many women are unaware of their pregnancy as they haven’t missed a period. A miscarriage during this time is often called a “chemical pregnancy” and may be mistaken for a regular menstrual period.
Weeks 4–12
If you know you’re pregnant and experience vaginal bleeding, abdominal or pelvic cramps, and back pain, you may be having a miscarriage. Additionally, the disappearance of common pregnancy symptoms like breast tenderness, nausea, and fatigue could be indicative.
Weeks 13–20
After week 13, vaginal bleeding, abdominal pain, and back pain are clear warning signs. Seek immediate medical attention if you experience any of these symptoms.
6. Strategies for Prevention
 Minimizing the Risk
Minimizing the Risk
Supplement with Folic Acid
Taking at least 400 mcg of folic acid daily can help prevent birth defects and significantly lower the chances of miscarriage.
Adopt a Healthy Lifestyle
Maintaining a healthy lifestyle is crucial. Limit alcohol and tobacco consumption and focus on eating a nutritious diet rich in fruits, vegetables, and whole foods.
Maintain a Healthy Weight
Obesity and being overweight increase the risk of complications. Strive for a stable BMI before and during pregnancy to reduce the likelihood of miscarriage.
Prevent Infections
Frequent handwashing can reduce the risk of respiratory infections and other illnesses. Stay up to date with vaccinations before planning a pregnancy to protect against diseases like measles, chickenpox, and hepatitis.
Manage Chronic Conditions
Address and manage any health conditions that could impact your pregnancy, such as hypertension and diabetes, to lower the risk.
Practice Safe Sex
Use protection during intercourse to prevent sexually transmitted infections, which can increase the chances of miscarriage.
7. Post-Miscarriage Care
 Taking Care of Yourself After a Miscarriage
Taking Care of Yourself After a Miscarriage
Rest and Recovery
It’s crucial to take time to rest and physically recover after a miscarriage. Avoid strenuous activities to prevent further exhaustion and potential gynecological issues.
Nutrition Is Key
Focus on replenishing your body with a balanced diet that includes proteins, carbohydrates, healthy fats, and vitamins. Your body loses a lot of energy and nutrients during a miscarriage, leading to exhaustion.
Emotional Wellbeing
Miscarriage can be emotionally challenging. Take time to process your emotions and gradually come to terms with your loss to support your mental health.
This article has provided an in-depth look at miscarriage, including common signs and effective prevention methods. Remember, knowledge and proactive measures can make a significant difference. Stay informed, and take care of yourself and your future baby!
Source: tamanhhospital.vn
Pregnant Women: What to Eat and What to Avoid for a Healthy Pregnancy
Pregnancy is an exciting yet delicate time, and it’s crucial for expecting mothers to be cautious about their diet. Our article today reveals the foods to avoid during pregnancy to lower the risk of miscarriage. We aim to provide valuable insights to help expecting mothers navigate their dietary choices and ensure a healthy journey towards motherhood.
The Great Pregnancy Myth: Debunking the Old Wives’ Tale of Eating Less for an Easier Birth
Pregnancy and nutrition are often a topic of discussion, with many old wives’ tales circulating. One such tale warns that overeating during pregnancy will lead to a difficult labor. The logic behind this is that the mother’s weight gain might not translate to adequate nutrition for the baby, and could even cause complications during childbirth. But is there any truth to this?